

Ayushman Bharat, a flagship scheme of Government of India, was launched as recommended by the National Health Policy 2017, to achieve the vision of Universal Health Coverage (UHC). This initiative has been designed to meet Sustainable Development Goals (SDGs) and its underlining commitment, which is to "leave no one behind."
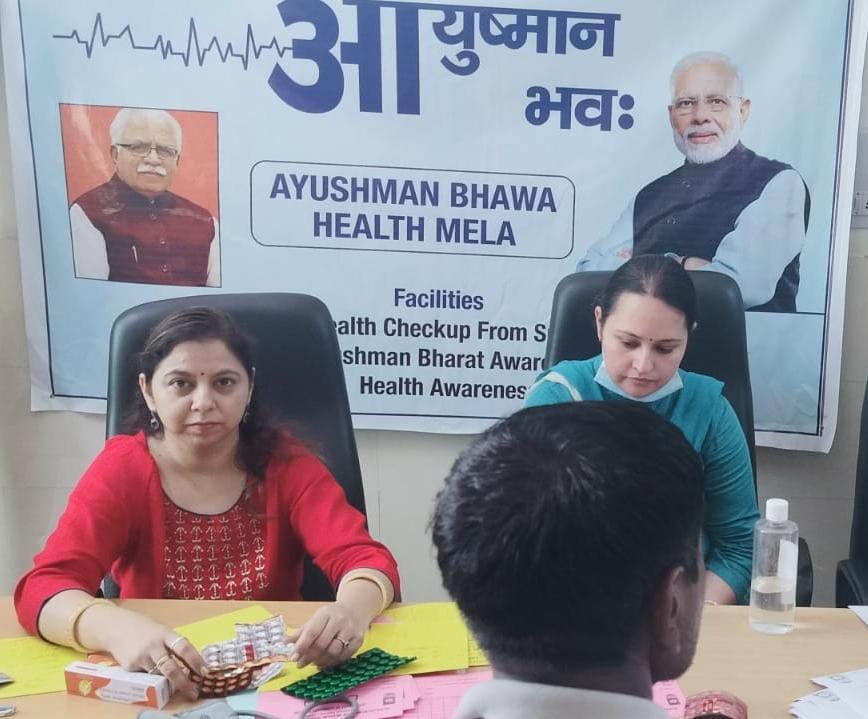
Al Falah School of Medical Sciences and Research Center has been empanelled with AYUSHMAN BHARAT SCHEME since 2018. Our Community Mediciine Department has been actively participating from finding the beneficiaries to awareness of the program and cashless treatment at Al Falah Hospital
Ayushman Bharat is an attempt to move from sectoral and segmented approach of health service delivery to a comprehensive need-based health care service. This scheme aims to undertake path breaking interventions to holistically address the healthcare system (covering prevention, promotion and ambulatory care) at the primary, secondary and tertiary level. Ayushman Bharat adopts a continuum of care approach, comprising of two inter-related components, which are -
Health and Wellness Centres (HWCs)
Pradhan Mantri Jan Arogya Yojana (PM-JAY)
The second component under Ayushman Bharat is the Pradhan Mantri Jan Arogya Yojana or PM-JAY as it is popularly known. This scheme was launched on 23rd September, 2018 in Ranchi, Jharkhand by the Hon’ble Prime Minister of India, Shri Narendra Modi.
Ayushman Bharat PM-JAY is the largest health assurance scheme in the world which aims at providing a health cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization to over 12 crores poor and vulnerable families (approximately 55 crore beneficiaries) that form the bottom 40% of the Indian population. The households included are based on the deprivation and occupational criteria of Socio-Economic Caste Census 2011 (SECC 2011) for rural and urban areas respectively. PM-JAY was earlier known as the National Health Protection Scheme (NHPS) before being rechristened. It subsumed the then existing Rashtriya Swasthya Bima Yojana (RSBY) which had been launched in 2008. The coverage mentioned under PM-JAY, therefore, also includes families that were covered in RSBY but are not present in the SECC 2011 database. PM-JAY is fully funded by the Government and cost of implementation is shared between the Central and State Governments.

PM-JAY is the world’s largest health insurance/ assurance scheme fully financed by the government.
It provides a cover of Rs. 5 lakhs per family per year for secondary and tertiary care hospitalization across public and private empanelled hospitals in India.
Over 12 crore poor and vulnerable entitled families (approximately 55 crore beneficiaries) are eligible for these benefits.
PM-JAY provides cashless access to health care services for the beneficiary at the point of service, that is, the hospital.
PM-JAY envisions to help mitigate catastrophic expenditure on medical treatment which pushes nearly 6 crore Indians into poverty each year.
It covers up to 3 days of pre-hospitalization and 15 days post-hospitalization expenses such as diagnostics and medicines.
There is no restriction on the family size, age or gender.
All pre–existing conditions are covered from day one.
Benefits of the scheme are portable across the country i.e. a beneficiary can visit any empanelled public or private hospital in India to avail cashless treatment.
Services include approximately 1,929 procedures covering all the costs related to treatment, including but not limited to drugs, supplies, diagnostic services, physician's fees, room charges, surgeon charges, OT and ICU charges etc.
Public hospitals are reimbursed for the healthcare services at par with the private hospitals.
Benefit cover under various Government-funded health insurance schemes in India have always been structured on an upper ceiling limit ranging from an annual cover of INR30,000 to INR3,00,000 per family across various States which created a fragmented system. PM-JAY provides cashless cover of up to INR5,00,000 to each eligible family per annum for listed secondary and tertiary care conditions. The cover under the scheme includes all expenses incurred on the following components of the treatment.
Medical examination, treatment and consultation
Pre-hospitalization
Medicine and medical consumables
Non-intensive and intensive care services
Diagnostic and laboratory investigations
Medical implantation services (where necessary)
Accommodation benefits
Food services
Complications arising during treatment
Post-hospitalization follow-up care up to 15 days